
There’s a lot of discussion these days about
gut health (link is external)—how a healthy gut can support overall
health,
and the ways a compromised gut may contribute to illness and disease.
We’re learning more about the complexity of the vast, dense, microbial
world of the human gut and its influence over immune health, hormone
balance,
brain function, and mental and physical equilibrium. What relationship exists between
sleep
and this microbial ecosystem within the body? Emerging science
demonstrates that there is a very real and dynamic connection between
the microbiome and sleep itself.
What is the microbiome?
The term
microbiome (link is external)
can mean a couple of different things. It is sometimes used to describe
the collection of all microbes in a particular community. In scientific
terms, the microbiome can also refer to the
genes
belonging to all the microbes living in a community. The microbiome is
often seen as a genetic counterpart to the human genome.
The genes that make up a person’s microbiome are far more numerous
than human genes themselves—there are roughly 100 times more genes in
the
human microbiome (link is external)
than in the human genome. This makes sense when you consider that there
are somewhere in the neighborhood of 100 trillion microbes living in
(and on) each of us—a combination of many different types, including
bacteria, fungi, viruses and other tiny organisms.
This vast array of microbial life lives on our skin and throughout
the body. The largest single collection of microbes resides in the
intestine—hence the attention to “gut” health. Here, trillions of
microscopic organisms live and die—and appear to exert a profound effect
on human health.
The microbiome and sleep
The human microbiota is a complicated, dynamic ecosystem within the
body. It appears to interact in some important ways with another
fundamental aspect of living—sleep. As with much about the microbiome,
there is a tremendous amount we don’t know about this interaction. That
said, there are some fascinating possible connections and shared
influences. Scientists investigating the relationship between sleep and
the microbiome are finding that this ecosystem may affect sleep and
sleep-related physiological functions in a number of ways—shifting
circadian rhythms (link is external), altering the body’s
sleep-wake cycle (link is external), and affecting
hormones that regulate sleep (link is external) and wakefulness. Our sleep, in turn, may affect the health and diversity of the human microbiome.
The microbial life within our bodies is in perpetual flux, with
microbes constantly being generated and dying. Some of this decay and
renewal naturally occurs during sleep. There’s no answer yet, however,
to the important question: What role does sleep itself play in
maintaining the health of the microbial world inside us, and which
appears to contribute so significantly to our health?
There are some important signs of a significant connection: We’ve seen research demonstrating that
circadian rhythm disruptions (link is external) can have negative effects on gut microbiota. (
More on this shortly.) There’s also evidence that the disordered breathing associated with
obstructive sleep apnea (OSA) (link is external), a common
sleep disorder,
may disrupt the health of the microbiome. Scientists put mice through a
pattern of disrupted breathing that mimicked the effects of OSA, and
found that the mice that lived with periods of OSA-like breathing for
six weeks showed significant changes to the diversity and makeup of
their microbiota.
Sleep and the gut-brain connection
A significant, fast-growing body of research illustrates the far-reaching effects of the
microbiome (link is external)
over brain function and brain health—as well as the influence of the
brain over gut health and the microbiome. This “gut-brain axis” appears
likely to have a profound influence over nearly every aspect of human
health and physiological function, including
sleep (link is external).
The constant communication and interplay between the gut and the
brain has the potential to influence and intersect with sleep directly
and indirectly. Let’s take a closer look at the ways that might occur:
Mood. Studies indicate that the health and balance of the
gut microbiota (link is external)
has a significant influence over our mood and emotional equilibrium.
Disruptions and an imbalance of gut microbes have been strongly
connected to
anxiety and depression (link is external). This has potentially significant implications for sleep, as both
anxiety and
depression can trigger or exacerbate
sleep disruptions (link is external).
Stress. Research is also revealing a complicated, two-way relationship between
stress and gut health (link is external) that also may exert influence over sleep and sleep architecture. Stress is an extremely common obstacle to healthy,
sufficient sleep (link is external).
Pain. Studies link gut health to pain perception, specifically for visceral pain. An
unhealthy microbiome (link is external)
appears to increase sensitivity to this form of pain. Like so many
others, this connection travels the communication pathway between the
gut and the brain. The connection between
sleep and physical pain (link is external) or discomfort is significant—the presence of pain can make falling asleep and staying asleep much more difficult.
Hormones.
Several hormones and neurotransmitters that play important roles in
sleep also have significant influence over gut health and function. The
intestinal microbiome produces and releases many of the same
neurotransmitters (link is external)—
dopamine, serotonin, and GABA among them—that help to regulate mood, and also help to promote sleep. Also:
- Melatonin, the “darkness hormone" essential to sleep and a
healthy sleep-wake cycle, also contributes to maintaining gut health.
Deficiencies in melatonin have been linked to increased permeability of
the gut—the so-called "leaky gut" (link is external)
increasingly associated with a range of diseases. Melatonin is produced
in the gut as well as the brain, and evidence suggests that intestinal melatonin (link is external) may operate on a different cyclical rhythm than the pineal melatonin generated in the brain.
- Cortisol is another hormone critical to the human sleep-wake cycle (link is external).
Rising levels of the hormone very early in the day help to promote
alertness, focus, and energy. Cortisol levels are influenced in several
ways within gut-brain axis (link is external):
The hormone is central to the stress and inflammatory response, and
also exerts an effect on gut permeability and microbial diversity. The
changes to cortisol that occur amid the interplay of the gut and brain
are likely to have an effect on sleep.
‘Circadian rhythms’ of the gut?
There is some pretty fascinating research connecting the gut microbiome to
circadian rhythms (link is external),
the 24-hour biological rhythms that regulate our sleep and wake cycles,
in addition to many other important physiological processes. A growing
number of studies now suggest that the vast and diverse microbial
ecosystem of the gut has its own daily rhythms. These microbiome rhythms
appear to be deeply entwined with
circadian rhythms (link is external)—research suggests that both
circadian and microbial rhythms (link is external)are capable of influencing and disrupting the other, with consequences for
health and sleep (link is external).
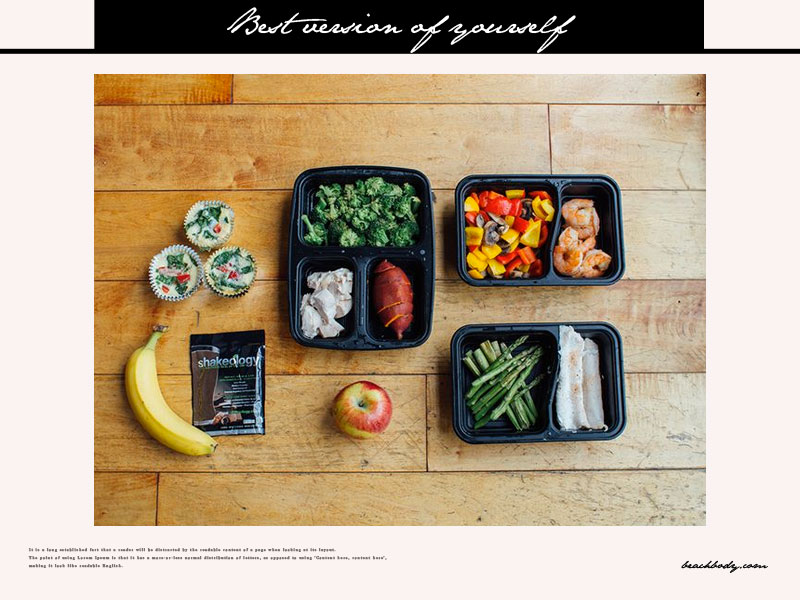
The
rhythms of gut microbes (link is external) are affected by
diet,
both the timing of our eating and the composition of the foods we
consume. A recent study found that mice eating a healthy diet generated
more beneficial gut microbes, and that the collective activity of
microbial life in the gut followed a daily—or diurnal—rhythm. That
rhythm, in turn, supported circadian rhythms in the animal. Mice fed a
high-fat, stereotypically “Western” diet, on the other hand, produced
less
optimal microbial life. The gut microbes of these mice did not adhere
to a daily rhythm themselves, and also sent signals that disrupted
circadian rhythms. These mice gained weight and became obese, while the
mice that ate healthfully did not.
Scientists bred a third group of mice without any gut microbes at
all. These mice had no signals to send from a gut microbiome. Circadian
disruption occurred in these mice—but they did not gain weight or suffer
metabolic disruption, even when fed the high-fat diet. This suggests a
couple of important conclusions. First, that microbial activity is key
to normal circadian function—and therefore to sleep. Second, that the
microbiome is a key player along with diet in the regulation of weight
and metabolism.
Circadian rhythms and microbiome: A two-way street
Research in humans has returned similar results: The human microbiome
appears to follow daily rhythms influenced by timing of eating and the
types of foods consumed, and to exert effects over circadian rhythms.
Research has also found that the relationship between these different
biological rhythms works both ways. Scientists have discovered that
disruptions to circadian rhythms (link is external)—the kind that occurs through
jet lag,
whether through actual travel or from “social” jet lag—disrupts
microbial rhythms and the health of the microbial ecosystem. People who
experience these changes to microbial rhythms as a result of circadian
disruption suffer metabolic imbalance, glucose intolerance, and weight
gain, according to research. And there’s preliminary evidence suggesting
that
gender
may play some role in the relationship of gut microbial health,
metabolism, and circadian function: a study using mice found that
females had more pronounced
microbiome rhythms (link is external) than males.
New understanding of circadian role in metabolism?
We’ve known for some time about the relationship of
sleep, circadian rhythms, and metabolic health (link is external). Disrupted sleep and misaligned circadian rhythms have been strongly tied to higher rates of
obesity and to metabolic disorders including
Type 2 diabetes. Our emerging knowledge of the microbiome and its
relationship to circadian function may in time deliver a deeper
understanding of how health is influenced by sleep and circadian
activity.
Science has really only just begun to delve into the world of the
microbiome and its relationship to sleep as well as health more broadly.
All the early signs suggest that this is a profoundly important area of
research; it will be fascinating to see where this takes us, and what
it means for sleep.
 Over the past 10 years, I’ve conducted studies designed to tap the practical wisdom
for living of the oldest Americans. Using a nationally representative
survey and in-depth interviews, I invited older people (mostly age 70
and above) to tell me what younger people should do—and not do—to live
happier, more fulfilling lives. I've especially loved it when the elders
have been definitive, as it was when we asked over 1,200 elders what
they would recommend to younger people looking for ways to make the most
of their lives. Many focused on this single action:
Over the past 10 years, I’ve conducted studies designed to tap the practical wisdom
for living of the oldest Americans. Using a nationally representative
survey and in-depth interviews, I invited older people (mostly age 70
and above) to tell me what younger people should do—and not do—to live
happier, more fulfilling lives. I've especially loved it when the elders
have been definitive, as it was when we asked over 1,200 elders what
they would recommend to younger people looking for ways to make the most
of their lives. Many focused on this single action:














 There’s a lot of discussion these days about
There’s a lot of discussion these days about 



















 It’s well established that physical activity—especially aerobic exercise like biking or running—helps people to sleep better.
It’s well established that physical activity—especially aerobic exercise like biking or running—helps people to sleep better.

