Early emotional trauma changes who we are, but we can do something about it.

If you’ve ever wondered why you’ve been struggling a little too hard for a little too long with chronic emotional and physical
health
conditions that just won’t abate, feeling as if you’ve been swimming
against some invisible current that never ceases, a new field of
scientific research may offer hope, answers, and healing insights.
In 1995, physicians Vincent Felitti and Robert Anda launched a
large-scale epidemiological study (link is external) that probed the child and adolescent histories of 17,000 subjects, comparing their
childhood
experiences to their later adult health records. The results were
shocking: Nearly two-thirds of individuals had encountered one or more
Adverse Childhood Experiences (ACEs)—a term Felitti and Anda coined to
encompass the chronic, unpredictable, and
stress-inducing events that some children face. These included growing up with a depressed or alcoholic parent; losing a parent to
divorce or other causes; or enduring chronic
humiliation, emotional neglect, or sexual or physical abuse. These forms of emotional
trauma went beyond the typical, everyday challenges of growing up. (
For stories of those who faced childhood adversity, see these videos on Laura (link is external) and John (link is external), two patients featured in my newest book, Childhood Disrupted: How Your Biography Becomes Your Biology, and How You Can Heal (link is external).)
The number of Adverse Childhood Experiences an individual had had
predicted the amount of medical care she’d require as an adult (link is external) with surprising accuracy:
- Individuals who had faced 4 or more categories of ACEs were
twice as likely to be diagnosed with cancer as individuals who hadn’t
experienced childhood adversity.
- For each ACE Score a woman had, her risk of being hospitalized with an autoimmune disease rose by 20 percent.
- Someone with an ACE Score of 4 was 460 percent more likely to suffer from depression than someone with an ACE Score of 0.
- An ACE Score greater than or equal to 6 shortened an individual’s lifespan by almost 20 years.
The ACE Study tells us that experiencing chronic, unpredictable
toxic stress in childhood predisposes us to a constellation of chronic
conditions in adulthood. But why? Today, in labs across the country,
neuroscientists are peering into the once inscrutable brain-body
connection, and breaking down, on a biochemical level, exactly how the
stress we face when we’re young catches up with us when we’re adults,
altering our bodies, our cells, and even our DNA.
What they’ve found (link is external) may surprise you.
Some of these scientific findings can be a little overwhelming to
contemplate. They compel us to take a new look at how emotional and
physical pain are intertwined. (For more on why I wrote about how ACEs
can change the way we see illness and how we do medicine, see this
video (link is external).)
[In Part I of this article, we’ll talk about the science of early
adversity and how it changes us. In Part II, we’ll talk about all the
science-based ways in which we can
reverse these changes, and get back to who it is we hope to be, so stay tuned for the good news.]
1. Epigenetic Shifts
When we’re thrust over and over again into stress-inducing situations during childhood or
adolescence,
our physiological stress response shifts into overdrive, and we lose
the ability to respond appropriately and effectively to future
stressors—10, 20, even 30 years later. This happens due to a process
known as gene methylation, in which small chemical markers, or methyl
groups, adhere to the
genes
involved in regulating the stress response, and prevent these genes
from doing their jobs. As the function of these genes is altered, the
stress response becomes re-set on “high” for life, promoting
inflammation and disease.
This can make us more likely to over-react to the everyday stressors
we meet in our adult life—an unexpected bill, a disagreement with a
spouse, or a car that swerves in front of us on the highway, creating
more inflammation. This, in turn,
predisposes (link is external) us to a host of chronic conditions, including autoimmune disease, heart disease, cancer, and
depression.
Indeed, Yale researchers recently found that children who’d faced
chronic, toxic stress showed changes “across the entire genome,” in
genes that not only oversee the stress response (link is external), but also in
genes implicated in a wide array of adult diseases (link is external).
This new research on early emotional trauma, epigenetic changes, and
adult physical disease breaks down longstanding delineations between
what the medical community has long seen as “physical” disease versus
what is “mental” or “emotional.”
2. Size and Shape of the Brain
Scientists have found that when the developing brain is chronically stressed, it releases a
hormone that actually
shrinks the size of the hippocampus (link is external), an area of the brain responsible of processing emotion and
memory
and managing stress. Recent magnetic resonance imaging (MRI) studies
suggest that the higher an individual’s ACE Score, the less gray matter
he or she has in other key areas of the brain, including the prefrontal
cortex, an area related to
decision-making and self-regulatory skills, and the amygdala, or
fear-processing
center. Kids whose brains have been changed by their Adverse Childhood
Experiences are more likely to become adults who find themselves
over-reacting to even minor stressors.
3. Neural Pruning
Children have an overabundance of neurons and synaptic connections;
their brains are hard at work, trying to make sense of the world around
them. Until recently, scientists believed that the pruning of excess
neurons and connections was achieved solely in a “use-it-or-lose-it”
manner, but a surprising new player in brain development has appeared on
the scene: non-neuronal brain cells—known as
microglia (link is external),
which make up one-tenth of all the cells in the brain, and are actually
part of the immune system—participate in the pruning process. These
cells prune synapses like a gardener prunes a hedge. They also engulf
and digest entire cells and cellular debris, thereby playing an
essential housekeeping role.
But when a child faces unpredictable, chronic stress of Adverse
Childhood Experiences, microglial cells “can get really worked up and
crank out neurochemicals that lead to neuroinflammation,” says Margaret
McCarthy, PhD, whose research
team
at the University of Maryland Medical Center studies the developing
brain. “This below-the-radar state of chronic neuroinflammation can lead
to changes that reset the tone of the brain for life.”
That means that kids who come into adolescence with a history of
adversity and lack the presence of a consistent, loving adult to help
them through it may become more likely to develop mood disorders or have
poor executive functioning and decision-making skills.
4. Telomeres
Early trauma can make children seem “older,” emotionally speaking,
than their peers. Now, scientists at Duke University; the University of
California, San Francisco; and Brown University have discovered that
Adverse Childhood Experiences may prematurely age children on a cellular
level as well. Adults who’d faced early trauma show greater erosion in
what are known as
telomeres (link is external)—the
protective caps that sit on the ends of DNA strands, like the caps on
shoelaces, to keep the genome healthy and intact. As our telomeres
erode, we’re more likely to develop disease, and our cells age faster.
5. Default Mode Network
Inside each of our brains, a network of neurocircuitry, known as the
“default mode network,” quietly hums along, like a car idling in a
driveway. It unites areas of the brain associated with memory and
thought integration, and it’s always on stand-by, ready to help us to
figure out what we need to do next. “The dense connectivity in these
areas of the brain help us to determine what’s relevant or not relevant,
so that we can be ready for whatever our
environment is going to ask of us,” explains Ruth Lanius, neuroscientist, professor of
psychiatry, and director of the
Post-Traumatic Stress Disorder (PTSD) Research Unit at the University of Ontario.
But when children face early adversity and are routinely thrust into a
state of fight-or-flight, the default mode network starts to go
offline; it’s no longer helping them to figure out what’s relevant, or
what they need to do next. According to Lanius, kids who’ve faced early
trauma have less connectivity in the default mode network—even decades
after the trauma occurred. Their brains don’t seem to enter that healthy
idling position—and so they may have trouble reacting appropriately to
the world around them.
6. Brain-Body Pathway
Until recently, it’s been scientifically accepted that the brain is
“immune-privileged,” or cut off from the body’s immune system. But that
turns out not to be the case, according to a
groundbreaking study (link is external)
conducted by researchers at the University of Virginia School of
Medicine. Researchers found that an elusive pathway travels between the
brain and the immune system via lymphatic vessels. The lymphatic system,
which is part of the circulatory system, carries lymph—a liquid that
helps to eliminate toxins, and moves immune cells from one part of the
body to another. Now we know that the immune system pathway includes the
brain.
The results of this study have profound implications for ACE
research. For a child who’s experienced adversity, the relationship
between mental and physical suffering is strong: the inflammatory
chemicals that flood a child’s body when she’s chronically stressed
aren’t confined to the body alone; they’re shuttled from head to toe.
7. Brain Connectivity
Ryan Herringa, neuropsychiatrist and assistant professor of child and
adolescent psychiatry at the University of Wisconsin, found that
children and teens who’d experienced chronic childhood adversity showed
weaker neural connections (link is external)
between the prefrontal cortex and the hippocampus. Girls also displayed
weaker connections between the prefrontal cortex and the amygdala. The
prefrontal-cortex-amygdala relationship plays an essential role in
determining how emotionally reactive we’re likely to be to the things
that happen to us in our day-to-day life, and how likely we are to
perceive these events as stressful or dangerous.
According to Herringa:
“If you are a girl who has had Adverse Childhood
Experiences and these brain connections are weaker, you might expect
that in just about any stressful situation you encounter as life goes
on, you may experience a greater level of fear and anxiety.”
Girls with these weakened neural connections, Herringa found, stood at a higher risk for developing
anxiety and
depression by the time they reached late adolescence. This may, in
part, explain why females are nearly twice as likely as males to suffer
from later mood disorders.
This science can be overwhelming, especially to those of us who are
parents. So, what can you do if you or a child you
love has been affected by early adversity? The good news is that, just as our scientific
understanding of how adversity affects the developing brain is growing, so is our scientific insight into
how we can offer the children we love resilient parenting (link is external),
and how we can all take small steps to heal body and brain. Just as
physical wounds and bruises heal, just as we can regain our muscle tone,
we can recover function in under-connected areas of the brain. The
brain and body are never static; they are always in the process of
becoming and changing.
 If you’ve ever wondered why you’ve been struggling a little too hard for a little too long with chronic emotional and physical health
conditions that just won’t abate, feeling as if you’ve been swimming
against some invisible current that never ceases, a new field of
scientific research may offer hope, answers, and healing insights.
If you’ve ever wondered why you’ve been struggling a little too hard for a little too long with chronic emotional and physical health
conditions that just won’t abate, feeling as if you’ve been swimming
against some invisible current that never ceases, a new field of
scientific research may offer hope, answers, and healing insights.
 Have you ever had the persistent feeling that you were out of place,
or felt a sense of sadness that you will never know what will happen to
your great-great-grandchildren? Some of these strange feelings have
names. See how many you have experienced:
Have you ever had the persistent feeling that you were out of place,
or felt a sense of sadness that you will never know what will happen to
your great-great-grandchildren? Some of these strange feelings have
names. See how many you have experienced: I’ve studied how pressure affects performance, and the best way to
manage it, for more than 20 years. I've interviewed elite athletes, Navy
SEALs, entrepreneurs, ER doctors and nurses, hedge fund managers, air
traffic controllers, and others who perform their best in pressure
moments more often than not. These individuals do not "rise to the
occasion," as conventional thinking instructs; rather they do their best
by depressurizing—lessening the pressure of the moment.
I’ve studied how pressure affects performance, and the best way to
manage it, for more than 20 years. I've interviewed elite athletes, Navy
SEALs, entrepreneurs, ER doctors and nurses, hedge fund managers, air
traffic controllers, and others who perform their best in pressure
moments more often than not. These individuals do not "rise to the
occasion," as conventional thinking instructs; rather they do their best
by depressurizing—lessening the pressure of the moment.
 As if we needed another reason to send more women to level-out STEM
fields, now we have it. New research from Indiana University Bloomington
shows that the interpersonal-stress from working in a male-dominated
field like engineering and construction can be as bad for women’s health as living in poverty.
As if we needed another reason to send more women to level-out STEM
fields, now we have it. New research from Indiana University Bloomington
shows that the interpersonal-stress from working in a male-dominated
field like engineering and construction can be as bad for women’s health as living in poverty. 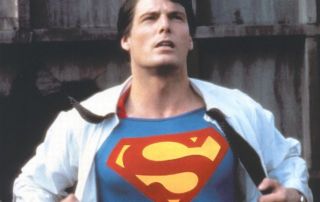 Every job comes with pressure but I think we’d all have to admit that
the pressure on Superman to meet his responsibilities would have to be
especially intense. Sure, he could always do the easy stuff—move faster
than a speeding bullet, leap tall buildings in a single bound, bend
steel in his bare hands, and change the course of mighty rivers. If he
were around today, though, he might be under even more pressure to
deliver results upholding truth, justice and the American way. Yet
Superman would never shrink from the challenge. He would never let
pressure sap his strength, as kryptonite would, or clog his memory,
downgrade his performance, or force him into a relationship
prematurely—all things that pressure routinely does to those of us born
under a yellow sun.
Every job comes with pressure but I think we’d all have to admit that
the pressure on Superman to meet his responsibilities would have to be
especially intense. Sure, he could always do the easy stuff—move faster
than a speeding bullet, leap tall buildings in a single bound, bend
steel in his bare hands, and change the course of mighty rivers. If he
were around today, though, he might be under even more pressure to
deliver results upholding truth, justice and the American way. Yet
Superman would never shrink from the challenge. He would never let
pressure sap his strength, as kryptonite would, or clog his memory,
downgrade his performance, or force him into a relationship
prematurely—all things that pressure routinely does to those of us born
under a yellow sun.